|
2型糖尿病早期是否应该采用胰岛素强化治疗呢?来自东弗吉尼亚医学院的 Gayle Nicholas Scott博士发表了自己的观点。
问题:早期胰岛素强化治疗是否可以缓解2型糖尿病?
2型糖尿病(T2DM)由胰岛素抵抗和(或)胰岛β细胞功能障碍导致胰岛素的相对不足,是一种伴有葡萄糖毒性的进展性疾病。
出现T2DM临床表现的患者β细胞功能障碍可能在15年前已经开始[2]。目前认为,T2DM是一种遗传和环境因素共同作用而形成的多基因遗传性复杂疾病,其特征是胰岛素抵抗、胰岛素分泌不足和肝糖输出增多。肥胖和久坐生活方式,尤其是2型糖尿病家族史均会促进疾病的进展。
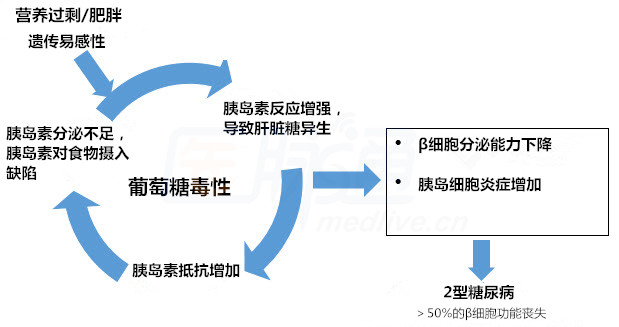
2型糖尿病的恶性循环[3,4]
目前指南推荐二甲双胍或其他口服降糖药作为疾病的初始治疗选择,随着疾病进展可添加其他药物,包括胰岛素[1]。胰岛素并不作为一线推荐药物使用,通常作为临床医生和患者控制血糖上升的最后选择。
一些研究表明,对于新诊断的T2DM患者,胰岛素强化治疗可阻断葡萄糖毒性或延缓疾病进展。胰岛素分泌周期缩短、葡萄糖生成增加及胰岛素抵抗等环节的中断可保护残存胰岛β细胞的功能、缓解高血糖,并可能改善疾病进展[3,4]。
英国前瞻性糖尿病研究(UKPDS)发现T2DM诊断后促使血糖快速正常化具有重要意义[5 ]。初始甘精胰岛素干预结局研究(ORIGIN)比较了初始治疗方案中加用胰岛素的有效性。参与者糖尿病前期病史平均时间为6.2年[6]。结果显示,尽管胰岛素增加低血糖风险且轻度增加参与者的体重,但是甘精胰岛素治疗相较于标准治疗组2型糖尿病患病风险降低28%。
几十年亚洲人群研究显示,对于新诊断的T2DM患者,通过外源性胰岛素短期强化治疗可缓解患者的胰腺自身压力并能有效延迟或预防糖尿病药物抗药性的出现[7-20]。大部分研究采用胰岛素泵给予基础胰岛素(一些采用每日多次皮下注射),一些研究加用餐时胰岛素。大部分研究治疗持续时间为2-4个周不等;一些研究治疗时间较长。在一项T2DM早期胰岛素强化治疗效果的荟萃分析显示:随访3个月,无抗糖尿病药参与者疾病缓解比例约为66%、12个月后为46%、24个月后为42%。[21]T2DM诊断后前两年是保证胰岛素强化治疗有效性的关键[22,23]。
诱导高血糖缓解和非抗糖尿病药物治疗下保持血糖正常水平的观点对于T2DM患者而十分诱人。尽管近三十年的研究已经发现T2DM患者采用胰岛素早期干预的获益性,但目前指南并不推荐或提及这一方法[1]。根据ORIGIN试验经济数据,高成本甘精胰岛素可长期应用解决T2DM新诊断的患者口服降糖药使用率较低的问题[24]。作者推测甘精胰岛素成本可通过糖尿病前期患者减少的医疗成本抵消,但是实际成本影响未知。
早期胰岛素强化干预对于糖尿病前期和新诊断的T2DM患者有可取之处,但胰岛素治疗费时且花费较高。目前来看,早期胰岛素强化治疗仍然是一个热门研究领域。
参考文献
1.American Diabetes Association. Standards of medical care in diabetes--2016. Diabetes Care. 2016;39(Suppl 1):S1-S106.
2.Mashitisho ML, Mashitisho BG. Early insulin therapy in patients with type 2 diabetes mellitus. J Endocrinol Metab Diab South Africa. 2016;21:13-15.
3.Halban PA, Polonsky KS, Bowden DW, et al. β-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care. 2014;37:1751-1758.
4.Hanefeld M, Monnier L, Schnell O, Owens D. Early treatment with basal insulin glargine in people with type 2 diabetes: lessons from ORIGIN and other cardiovascular trials. Diabetes Ther. 2016;7:187-201.
5.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405-412.
6.ORIGIN Trial Investigators, Gerstein HC, Bosch J, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367:319-328.
7.llkova H, Glaser B, Tunçkale A, Bagriaçik N, Cerasi E. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Care. 1997;20:1353-1356.
8.Park S, Choi SB. Induction of long-term normoglycemia without medication in Korean type 2 diabetes patients after continuous subcutaneous insulin infusion therapy. Diabetes Metab Res Rev. 2003;19:124-130.
9.Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care. 2004;27:1028-1032.
10.Torella R, Salvatore T, Cozzolino D, Giunta R, Quatraro A, Giugliano D. Restoration of sensitivity to sulfonylurea after strict glycaemic control with insulin in non-obese type 2 diabetic subjects. Diabetes Metab. 1991;17:443-447.
11.Li Y, Xu W, Liao Z, et al. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of beta-cell function. Diabetes Care. 2004;27:2597-2602.
12.Scarlett JA, Gray RS, Griffin J, Olefsky JM, Kolterman OG. Insulin treatment reverses the insulin resistance of type II diabetes mellitus. Diabetes Care. 1982;5:353-363.
13.Andrews WJ, Vasquez B, Nagulesparan M, et al. Insulin therapy in obese, non-insulin-dependent diabetes induces improvements in insulin action and secretion that are maintained for two weeks after insulin withdrawal. Diabetes. 1984;33:634-642.
14.Chen HS, Wu TE, Jap TS, Hsiao LC, Lee SH, Lin HD. Beneficial effects of insulin on glycemic control and beta-cell function in newly diagnosed type 2 diabetes with severe hyperglycemia after short-term intensive insulin therapy. Diabetes Care. 2008;31:1927-1932.
15.Weng J, Li Y, Xu W, et al. Effect of intensive insulin therapy on beta cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet. 2008;371:1753-1760.
16.Chen H, Ren A, Hu S, Mo W, Xin X, Jia W. The significance of tumor necrosis factor-alpha in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Res Clin Pract. 2007;75: 327-332.
17.Zhao QB, Wang HF, Sun CF, Ma AQ, Cui CC. [Effect of short-term intensive treatment with insulin pump on beta cell function and the mechanism of oxidative stress in newly diagnosed type 2 diabetic patients]. Nan Fang Yi Ke Da Xue Xue Bao. 2007;27:1878-1879 (in Chinese).
18.Chen A, Huang Z, Wan X, et al. Attitudes toward diabetes affect maintenance of drug-free remission in patients with newly diagnosed type 2 diabetes after short-term continuous subcutaneous insulin infusion treatment. Diabetes Care. 2012;35:474-481.
19.Liu L, Ke W, Wan X, et al. Insulin requirement profiles of short-term intensive insulin therapy in patients with newly diagnosed type 2 diabetes and its association with long-term glycemic remission. Diabetes Res Clin Pract. 2015;108:250-257.
20.Kramer CK, Choi H, Zinman B, Retnakaran R. Glycemic variability in patients with early type 2 diabetes: the impact of improvement in β-cell function. Diabetes Care. 2014;37:1116-1123.
21.Kramer CK, Zinman B, Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:28-34.
22.Kramer CK, Zinman B, Choi H, Retnakaran R. Predictors of sustained drug-free diabetes remission over 48 weeks following short-term intensive insulin therapy in early type 2 diabetes. BMJ Open Diabetes Res Care. 2016;4:e000270.
23.Stein CM, Kramer CK, Zinman B, Choi H, Opsteen C, Retnakaran R. Clinical predictors and time course of the improvement in β-cell function with short-term intensive insulin therapy in patients with type 2 diabetes. Diabet Med. 2015;32:645-652.
24.Lamy A, Tong W, Jung H, et al; ORIGIN Investigators. Cost implications of the use of basal insulin glargine in people with early dysglycemia: the ORIGIN trial. J Diabetes Complications. 2014;28:553-558.
医脉通编译自:Early Intensive Insulin in Type 2 Diabetes.Medscape.January 12, 2017.
来源为“医脉通”
|